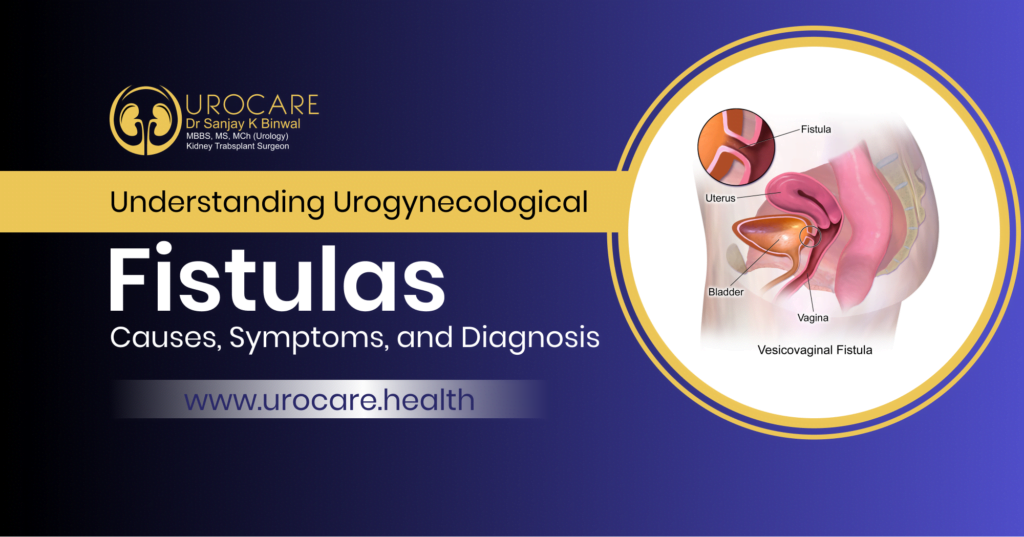
Urogynecological fistulas are a distressing and often misunderstood condition that affects many individuals, particularly women. These fistulas occur when abnormal connections develop between the bladder, urethra, vagina, or rectum, leading to the unintended passage of urine or feces. The causes of urogynecological fistulas can vary, including obstetric injuries, gynecological surgeries, or chronic inflammation. This article aims to provide a comprehensive understanding of urogynecological fistulas by exploring their causes, symptoms, and available diagnostic methods. Keep on reading ill the end to know about all of this in detail!
Common Causes of Urogynecological Fistulas:
Obstetric Causes:
Pregnancy and childbirth can sometimes be the culprits behind urogynecological fistulas. The pressure and trauma from labor can lead to these unwanted connections forming, and well, they really don’t know when to quit.
Gynecological Surgeries:
Let’s give a round of applause to gynecological surgeries, such as hysterectomies or removal of uterine fibroids. While they can provide relief from certain conditions, they can also pave the way for these unwanted fistulas to make themselves at home. Talk about adding insult to injury!
Chronic Inflammation and Infections:
Chronic inflammation or infections in the pelvic area can also be guilty parties. They can weaken the tissues, making them more susceptible to developing fistulas. It’s like the perfect storm brewing down there, and nobody wants to deal with that level of chaos.
Surgical Complications:
Fistulas can develop as a result of surgical procedures involving the pelvic region, such as hysterectomy, colorectal surgery, or pelvic organ prolapse repair. In some cases, accidental injury to nearby organs can occur during surgery, leading to fistula formation.
Infections:
Infections in the pelvic area, such as pelvic inflammatory disease (PID), can lead to tissue damage and subsequent fistula formation if left untreated.
Radiation Therapy:
Radiation therapy used to treat cancers in the pelvic area can cause damage to healthy tissues and increase the risk of developing urogynecological fistulas.
Inflammatory Bowel Disease (IBD):
Conditions like Crohn’s disease and ulcerative colitis, which are types of IBD, can lead to chronic inflammation and ulceration in the gastrointestinal tract. This inflammation can increase the risk of fistula formation between the bowel and vagina.
Pelvic Inflammatory Conditions:
Chronic pelvic inflammatory conditions, such as chronic pelvic inflammatory disease, can weaken pelvic tissues and contribute to the development of fistulas.
Trauma or Injury:
Trauma or injury to the pelvic region, whether from accidents or other causes, can damage the tissues and create an abnormal connection between the vagina and nearby organs.
Foreign Bodies:
In rare cases, the presence of foreign bodies in the vaginal canal can lead to pressure or erosion of adjacent structures, potentially causing a fistula.
Symptoms and Effects of Urogynecological Fistulas:
Urinary Incontinence:
One of the hallmark symptoms of urogynecological fistulas is urinary incontinence, where urine involuntarily leaks from the vagina. This can range from mild to severe and may occur during activities like laughing, coughing, sneezing, or even just standing up.
Fecal Incontinence:
Fistulas involving the rectum can lead to fecal incontinence, causing stool to pass into the vagina unexpectedly. This can be embarrassing and emotionally distressing for affected individuals.
Vaginal Discharge:
Patients with urogynecological fistulas may experience abnormal vaginal discharge that can be foul-smelling due to the presence of urine or feces. This discharge can lead to discomfort and hygiene issues.
Recurrent Urinary Tract Infections (UTIs):
The continuous leakage of urine into the vaginal canal can increase the risk of recurrent UTIs. These infections can cause pain, discomfort, and require repeated antibiotic treatments.
Skin Irritation and Infections:
Constant exposure to urine or feces can irritate the skin in the genital and perianal area, potentially leading to skin infections, sores, and discomfort.
Psychological and Emotional Distress:
Living with urogynecological fistulas can have a profound emotional impact on individuals. The embarrassment, social stigma, and disruption of daily life can lead to anxiety, depression, and a decreased overall quality of life.
Social Isolation:
Many individuals with urogynecological fistulas may withdraw from social activities and relationships due to embarrassment and fear of leakage episodes. This social isolation can further contribute to emotional distress.
Diagnosing Urogynecological Fistulas
Medical History and Physical Examination:
The journey towards diagnosing these fistulas usually starts with a good old-fashioned medical history and a thorough physical examination. Your doctor will want to know all about your symptoms and any previous surgeries or infections that might have tipped the scales in favor of these pesky fistulas.
Imaging and Diagnostic Tests:
To get a better look at what’s going on, imaging and diagnostic tests come into play. This might involve ultrasound, MRI, or CT scans that can help identify the exact location and extent of the fistula. It’s like going on a little adventure inside your body, but with high-tech equipment instead of a treasure map.
Specialized Tests for Fistula Identification:
In some cases, specialized tests might be needed to pinpoint the fistula. This can include filling your bladder with a dye and observing if it leaks into the vagina or using a flexible tube to examine the rectum. Don’t worry, they won’t use a periscope or a magnifying glass; it’s a bit more high-tech than that.
Now that we’ve shed some light on the causes, symptoms, and diagnosis of urogynecological fistulas, it’s time to get the help you need and send those unwanted connections packing. Remember, you’re not alone, and with the right treatment, you can bid farewell to these uninvited guests and reclaim control over your own body.
Understanding urogynecological fistulas is crucial for both healthcare professionals and individuals affected by this condition. By recognizing the causes, symptoms, and diagnostic approaches, early intervention and appropriate treatment can be initiated, leading to improved outcomes and quality of life. While urogynecological fistulas can present significant challenges, advancements in surgical techniques and supportive care offer hope for affected individuals. You can reach Urologist in Jaipur and seek the treatment right away. You will be able to find out answers for all the queries that might be in your head regarding the condition you are going through.
Are you affected by the Fistulas problem? Consult with Dr. Sanjay K. Binwal, a leading urologist in Jaipur. Book a scheduled call with Dr. Sanjay K. Binwal. Looking for Urogynecological Fistula treatment in Jaipur must book an appointment with Dr. Sanjay K Binwal, He is one of the top-rated Uro-Gynecologist in Jaipur. Book an appointment now at 8820269369.
FAQ
1. How common are urogynecological fistulas?
Urogynecological fistulas are relatively rare, but they can occur in individuals of any age or background. The prevalence of urogynecological fistulas varies depending on the underlying causes and population studied. Obstetric fistulas, for example, are more common in developing countries with limited access to proper obstetric care.
2. Can urogynecological fistulas be prevented?
While not all urogynecological fistulas can be prevented, there are measures that can reduce the risk. Good obstetric practices, such as skilled delivery attendance and appropriate use of instruments during childbirth, can minimize the occurrence of obstetric fistulas. In gynecological surgeries, adherence to surgical guidelines and meticulous technique can help prevent iatrogenic fistulas. Additionally, managing chronic inflammation and infections promptly can reduce the risk of developing fistulas.
3. What treatment options are available for urogynecological fistulas?
The treatment of urogynecological fistulas depends on various factors, including the type, size, and location of the fistula, as well as the individual’s overall health. Conservative management approaches, such as bladder catheterization and wound care, may be used for smaller fistulas. Surgical interventions, including fistula repair or reconstructive procedures, are often necessary for larger or more complex fistulas. The choice of treatment is determined through a careful assessment by a healthcare professional specializing in urogynecology.
4. Are there support groups or resources available for individuals with urogynecological fistulas?
Yes, there are support groups and resources available for individuals living with urogynecological fistulas. These support networks provide a platform for individuals to connect, share experiences, and seek emotional support. Additionally, healthcare professionals and organizations specializing in urogynecology can provide valuable information and guidance on managing the physical, emotional, and social aspects of living with a urogynecological fistula.